Staff at all levels must know when they need to seek additional help because a participant is experiencing mental health or other challenges. This can be hard to navigate, as both coaches and therapists focus on helping participants identify goals and transform their lives. However, it’s important for coaches to watch for signs of when you should refer a participant for more intensive counseling or mental health services.
An active mental illness, substance abuse, or domestic violence situation may require a referral to fully support the participant. There are no hard rules on when and how to address these issues in a way that respects the relationship with the participant. If as a coach you begin to sense that certain topics or issues are beyond your ability to provide help, you should bring up the idea of a referral with the participant and together decide what would be most helpful.
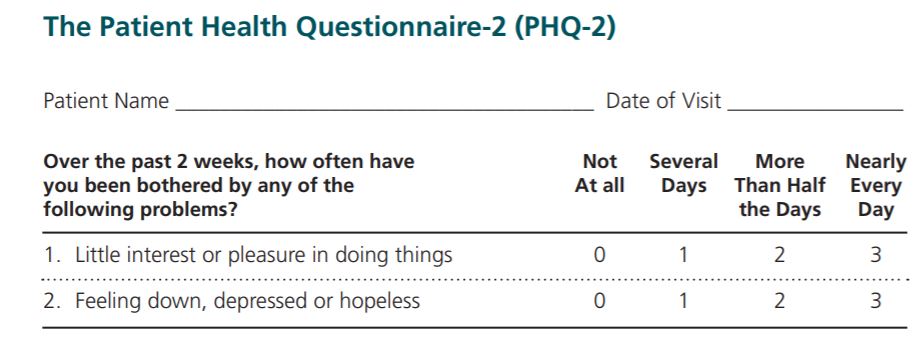
The Patient Health Questionnaire-2 (PHQ-2)
A commonly used tool for mental health is the Patient Health Questionnaire-2. These two questions are a first step to determine if further consultation or referrals might be needed. The scoring for the PHQ-2 goes from 0 to 6. Roughly, anyone scoring a 3 or above should have further assessment. Many participants do not test for a depressive disorder, but still have symptoms severe enough to affect their lives and the outcomes of their children. Follow the lead of the participant in identifying what would be most helpful. More information on the PHQ can be found at the Center for Quality Assessment and Improvement in Mental Health (CQAIMH).
Top 10 Indicators For When to Refer Participant to a Mental Health Professional
If your participant:
- Is exhibiting a decline in his/her ability to experience pleasure and/or an increase in being sad, hopeless, and helpless (example: The participant may make comments about “why bother” or “what’s the use.”)
- Has intrusive thoughts or is unable to concentrate or focus (example: Your participant reports that she has many thoughts inside her head and she can’t get them to slow down.)
- Is unable to get to sleep or awakens during the night and is unable to get back to sleep, or sleeps excessively (example: Your participant begins talking about not being able to get to sleep or how he just wants to sleep all the time.)
- Has a change in appetite, decrease in appetite, or increase in appetite
- Is feeling guilty because others have suffered or died (example: Your participant reports that he feels guilty because he is alive or has not been injured.)
- Has feelings of despair or hopelessness (example: According to your participant, nothing in life is okay.)
- Is being hyper-alert or excessively tired (example: Your participant reports that it feels like she always has to be on guard.)
- Has increased irritability or outbursts of anger (example: Your participant becomes increasingly belligerent or argumentative with you or other people.)
- Has impulsive and risk-taking behavior (example: Your participant reports doing things such as going on a buying spree without thinking about the consequences of the behavior.)
- Has thoughts of death and/or suicide (example: Your participant makes comments that to die right now would be OK with them.)
Adapted from Financial Coaching: Helping Clients Reach Their Goals. (2011). Washington, DC: NeighborWorks America.
Mandatory Reporting Laws
Some states have mandatory reporting laws, especially around issues of attempted suicide, child abuse, and neglect. Research your state reporting laws prior to working with participants. If those issues arise while coaching a participant, follow your state’s guidelines.
The Prosperity Agenda provides these resources as the designated national administrator of Family-Centered Coaching.

